The Matka of Statin Intolerance
Many of the so-called side effects of statins are nothing but a nocebo effect.

I was speaking to a colleague, who works in the pharma industry, and has also worked in healthcare service delivery. His brother had calcium in the coronary arteries, which is a good risk predictor for the likelihood of coronary artery disease. A calcium score above 100 generally implies the need to start drugs such as statins, which not only lower the cholesterol levels in the body, but also work on the plaques in the coronary arteries and stabilize them, preventing them from rupturing and causing “heart attacks”.
He mentioned that the new guidelines are very clear that lipid levels are no longer important and statins are no longer needed. It was something he had read in the “Encyclopedia of WhatsApp” and despite being someone who is a little conversant with healthcare issues, had fallen prey to misinformation.
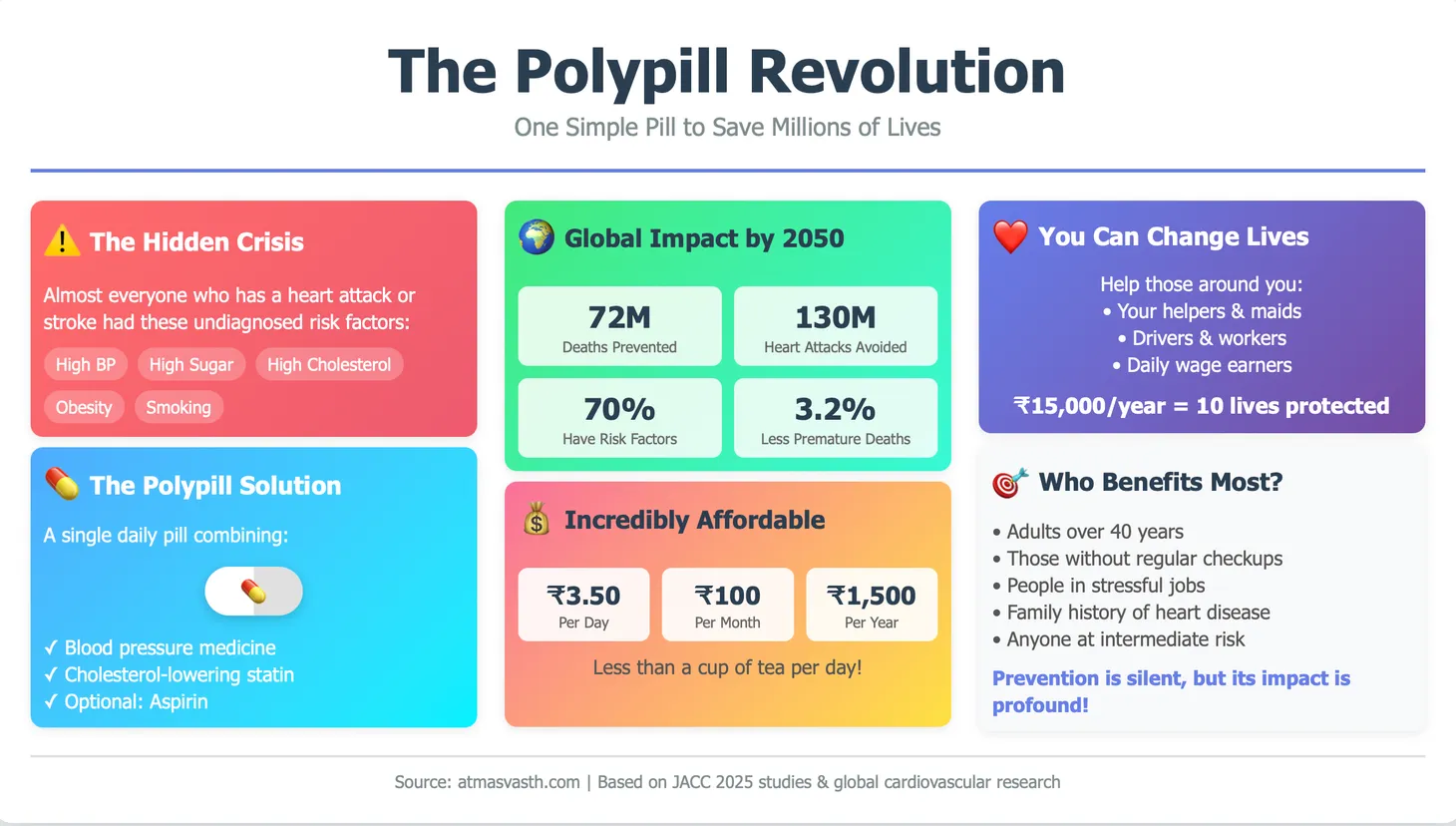
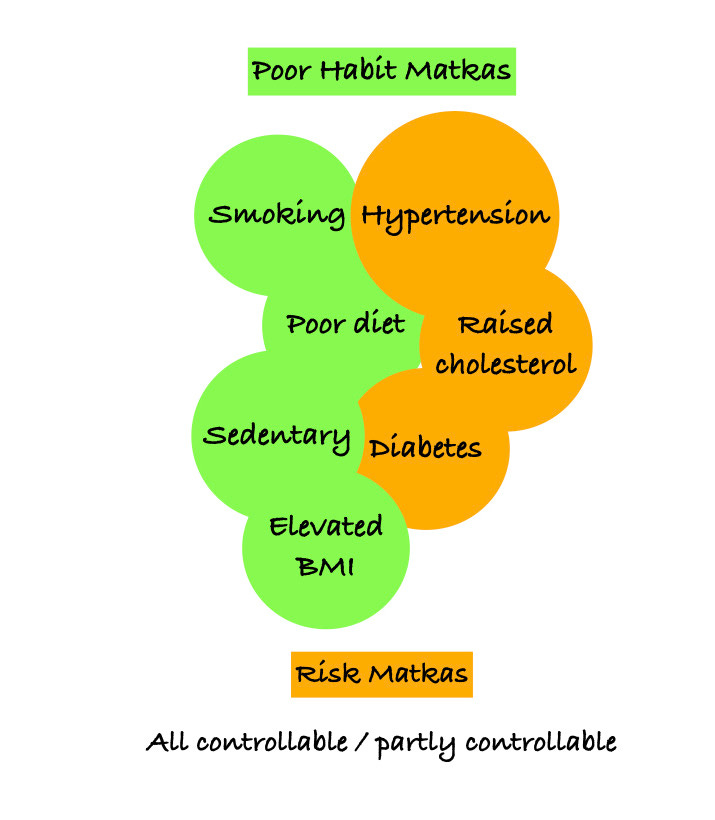
Dr. Vera Bittner [1] in a perspective piece on the new 2019 ACC/AHA Guidelines for the Primary Prevention of Cardiovascular Disease [2], succinctly puts down the matkas of cardiovascular risk. “much of the cardiovascular disease burden and mortality can be traced back to 4 adverse health behaviors (smoking, poor diet, elevated body mass index, and sedentary lifestyle) and 3 major risk factors (hypercholesterolemia, hypertension, and diabetes)”. Most of these are controllable or partly controllable matkas.
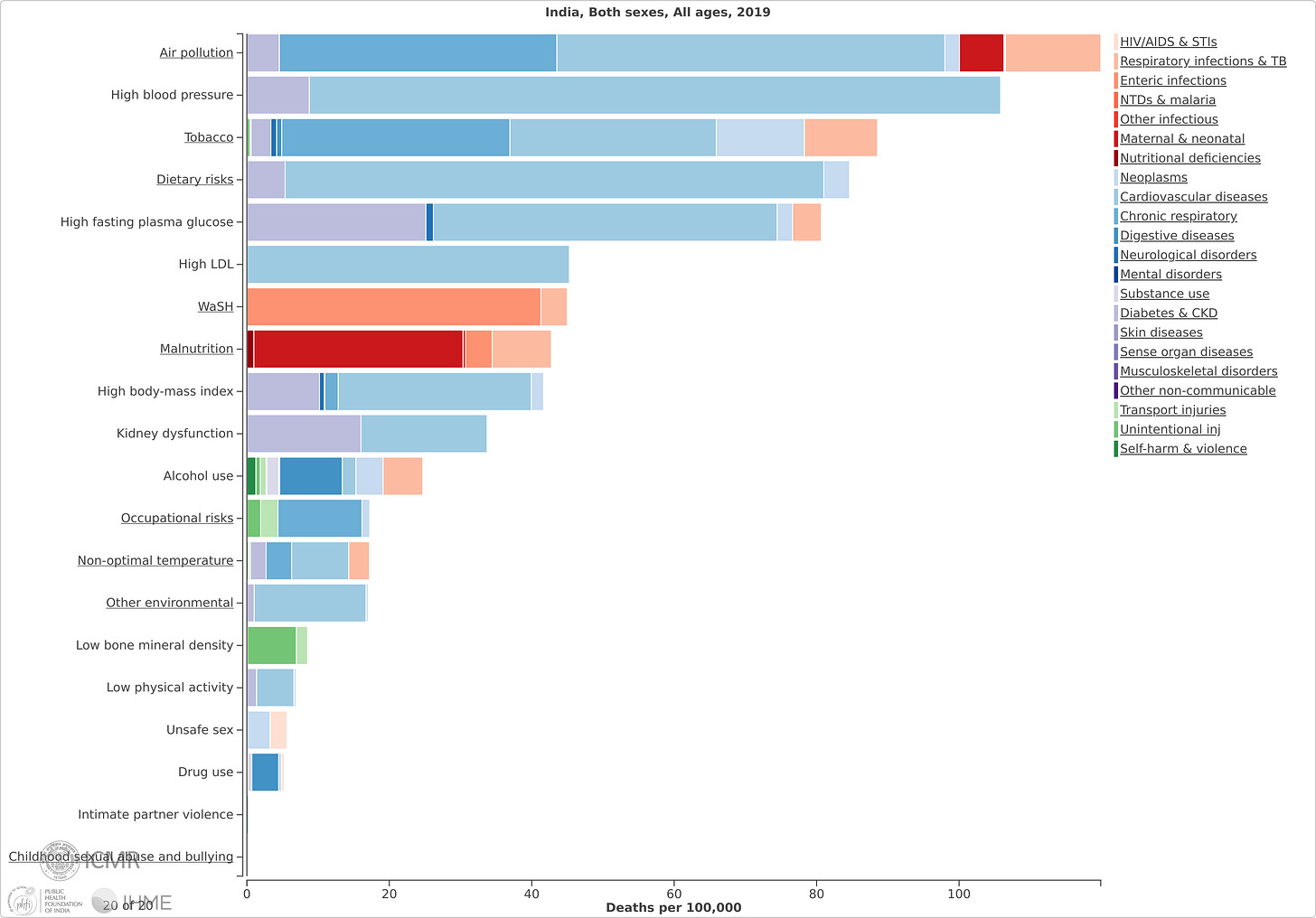
Globally, high LDL cholesterol (LDL-C) is the third most important cause of cardiovascular disease (CVD) [3].
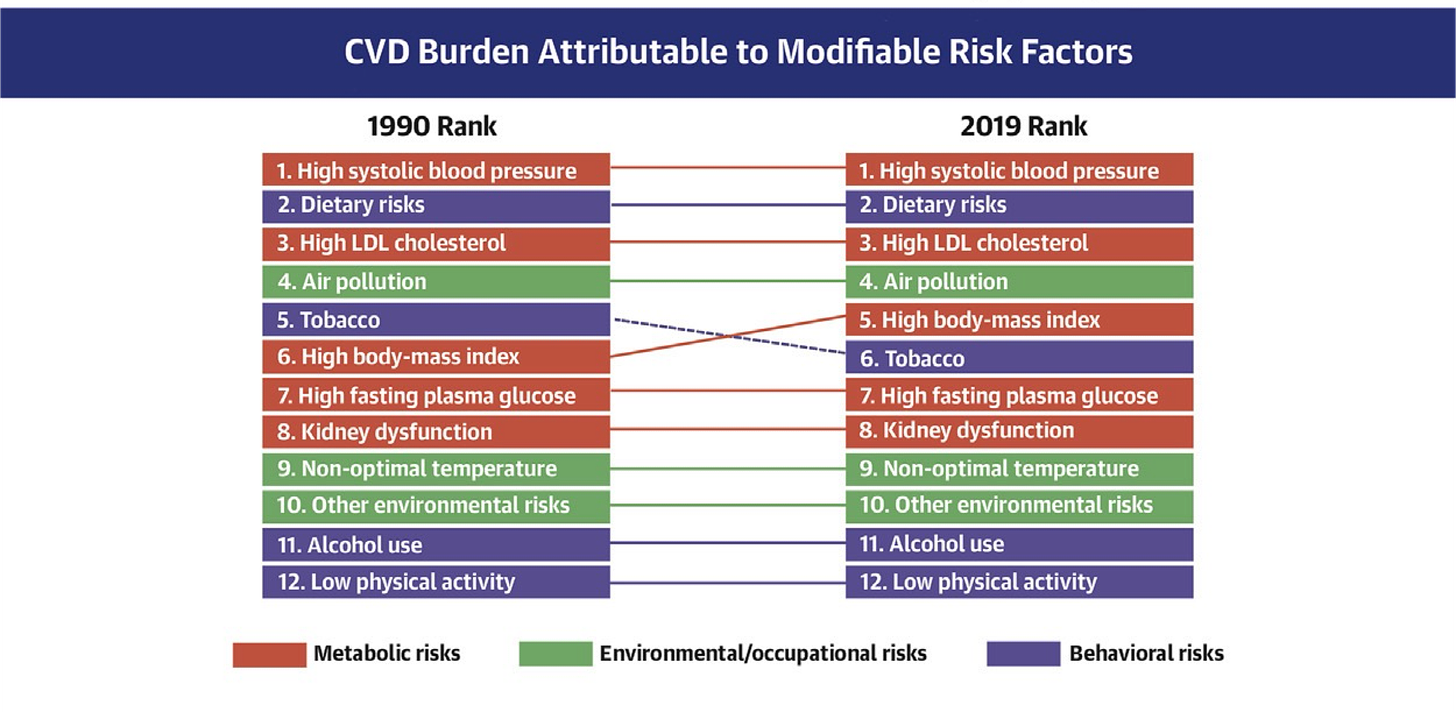
In India, in 2019, high LDL-C levels were the sixth commonest cause of estimated deaths (average of 630,000, around 6.7% of all deaths with an average rate of 45% per 100,000) [4].
The lower the LDL-C, the lower is the risk of a cardiac event [image adapted from 5].
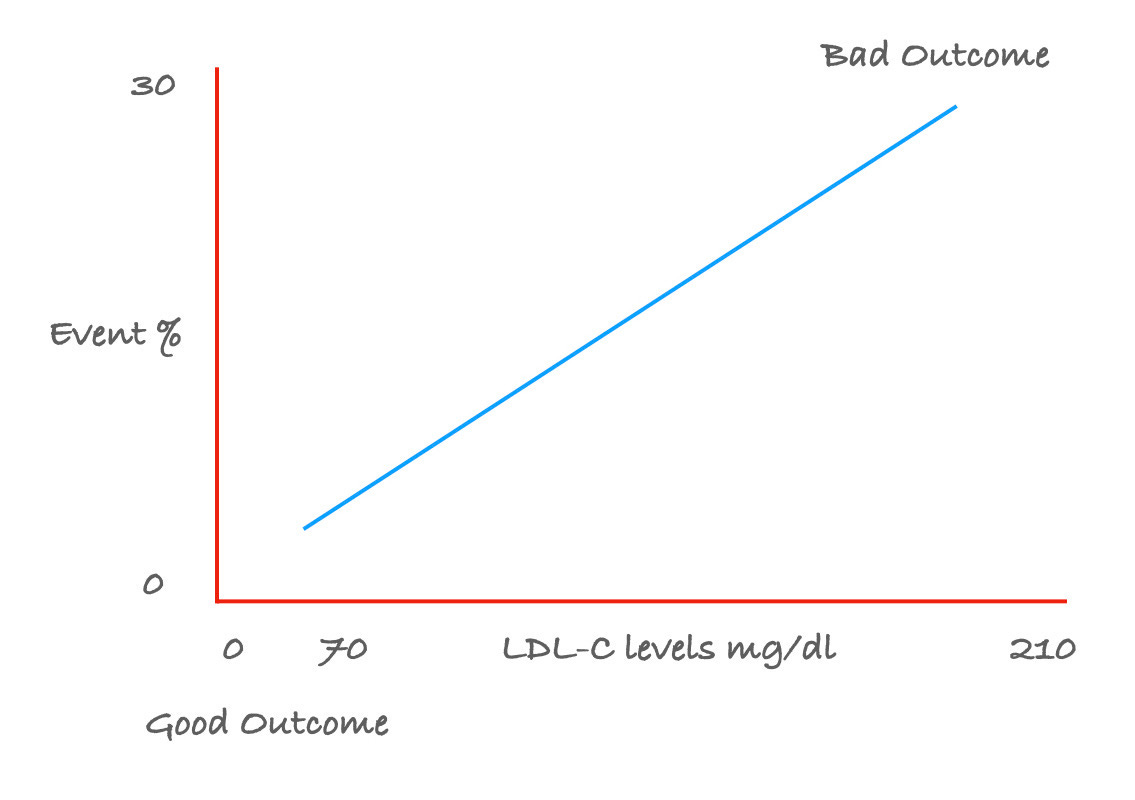
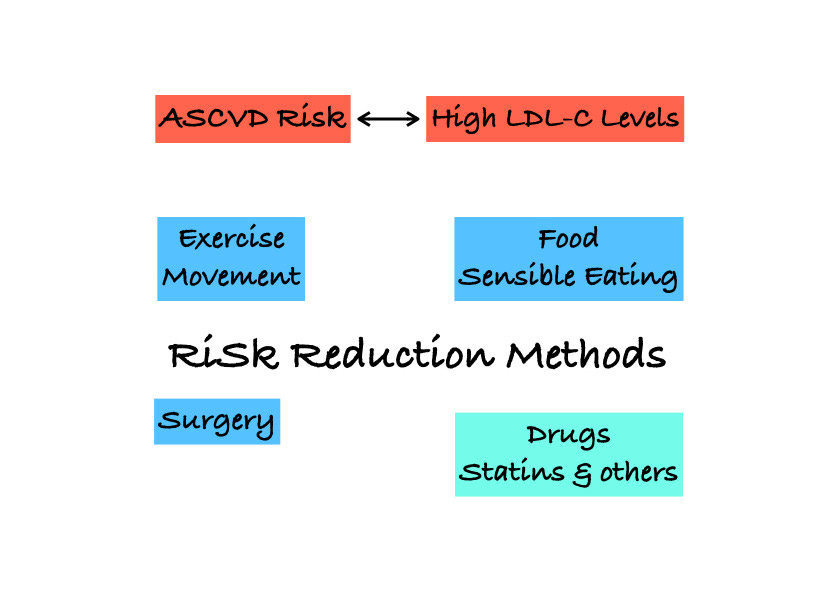
Lowering of LDL-C levels can be achieved with food control (sensible eating, diets), exercise, drugs and surgery (bariatric, ileal bypass). Ideally, the LDL-C level should be below 70 mg/dl, especially if there is any level of risk for atherosclerotic cardiovascular disease (ASCVD) (to be calculated using clinical and laboratory parameters) and between 70-100 mg/dl, if the ASCVD risk is low.
If non-drug therapies can keep the LDL-C level below 70 mg/dl and definitely below 100 mg/dl, great…else it becomes necessary to use drugs to control the LDL-C levels. Of the various drugs available, statins have been proven to be the best class of drugs for controlling and lowering LDL-C levels [6]. If the ASCVD risk is high, even with a healthy lifestyle incorporating movement and sensible eating, statins are still recommended to not just control the LDL-C levels, but also to stabilize plaques within the coronary arteries [7].
This post is free to read, but you will need to subscribe with your email ID to read the rest of the post and to listen to the accompanying audio/podcast.
Statins have been around for 35 years and have a high safety profile [8]. Unfortunately, as with my colleague, statins are highly underutilized for a variety of reasons, including misinformation related to their side-effects, both short-term and long-term. There are many websites and articles that have tried to deal with this [9] but have not been successful in tackling “statin-antipathy”.
How does this matka affect us? If we are at risk for cardiovascular disease (and remember we can measure our own risk) and we don’t take statins for primary prevention (i.e. we haven’t yet had a cardiac event), then we are doing ourselves a significant disservice not using a powerful tool that can reduce our chance of being adversely affected by a cardiac event (heart attack) or a stroke (brain attack). In our quest to be atmasvasth, not taking statins when needed reduces our healthspan and lifespan.
Multiple studies have shown that the incidence of side effects is extremely low [10]. Typically, treatment of 10,000 patients for 5 years with a standard statin, would be expected to cause 5 cases of myopathy, 50-100 cases of new diabetes and 5-10 hemorrhagic strokes.
What most of us worry about though is “statin intolerance” (a combination of muscle weakness, brain fog and a general “not feeling very good” situation), which is a subjective adverse experience. If we think we have “statin intolerance”, it is likely that we will complain about this to friends, family and colleagues, which in turn will put off many other people who would otherwise benefit from statins, from even starting statins.
This piece is about an interesting study [11], recently reported in the New England Journal (NEJM) where Frances Woodand her colleagues gave 60 patients four bottles each of atorvastatin and placebo and four empty bottles, to be used for 1 month each in a random sequence, for 12 months. 49 patients completed this study, where they had to record their symptoms daily using a smartphone app. The study found a nocebo ratio (i.e. ratio of symptom intensity with placebo vs ratio of symptom intensity with statin) of 2.2, which then was brought down to 0.9 on re-analysis by another statistician. A 90% nocebo rate however is still very significant.
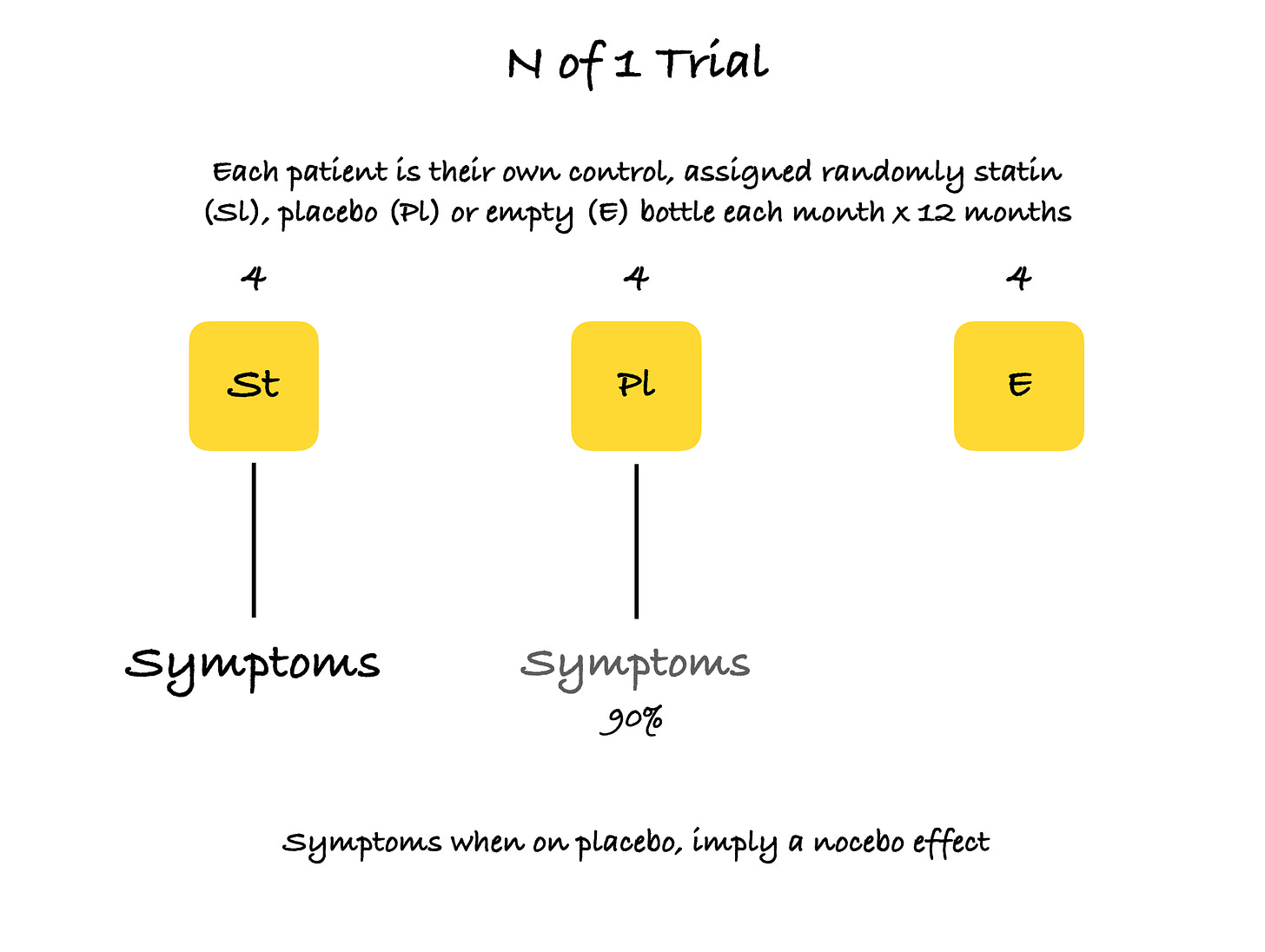
These statements are excerpted from the Supplementary material accompanying this article, for those interested in some more detail. “24 (49%) of the 49 participants who completed the trial stopped tablets early due to intolerable side effects for at least one month of the trial, with 71 stoppages in total. Of the 71 stoppages, 31 were during placebo months and 40 were during statin months. 6 months after completing the trial, 30 out of 60 entrants (50%) had successfully restarted statins.”
The nocebo effect is defined as one where a person gets symptoms that one would otherwise get with a drug, even if all we are given is a placebo [12]. Trials of the nocebo effect are important, because they tell us that many symptoms experienced with certain medications, may just be because our minds have been primed to experience these reactions because of what we have read or heard. A few years ago, I wrote about a sham trial done with people who lived near cellphone towers and seemed to experience ill-health and poor sleep [13]. In this trial [14], people were randomly exposed to cellphone towers that were either active or deactivated and no difference was found in the reported sleep problems, suggesting a significant nocebo effect related to our belief of an apparent adverse effect of cellphone tower related electromagnetic radiation.
I have a high ASCVD risk. I take rosuvastatin and my LDL levels have been below 70 mg/dl for the last 2 years. Though I exercise daily (running, strength training) and have controlled eating habits, I could not get my LDL-C levels below 150 mg/dl for years. I tried atorvastatin a decade ago and whether this was coincidental or not, landed up with a flu-like syndrome the next day. It took me 10 years to restart statins, which I finally did on the advice of a peer and another senior physician and I have had no problems since.
So how does all of this affect us and our matkas? If we are at risk for CVD (and we can measure our own risk ourselves) and/or have high LDL-C levels that need to be lowered, and we don’t take statins because we have “heard” that they are not “good”, perhaps we may want to rethink our situation and reconsider starting statins, working in concert with our regular/trusted physician in the initial stages.
In future posts, we will talk about how to understand all the other cardiovascular risk factors and matkas and how to take control and manage as many of these as possible, ourselves.
Footnotes
1. Bittner V. The New 2019 AHA/ACC Guideline on the Primary Prevention of Cardiovascular Disease. Circulation. 2020 Dec 22;142(25):2402–4.
2. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. Journal of the American College of Cardiology. 2019 Sep;74(10):e177–232.
3. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. Journal of the American College of Cardiology. 2020 Dec;76(25):2982–3021.
4. https://vizhub.healthdata.org/gbd-compare/india#
5. LaRosa JC et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 2005; 352: 1425–1435.
6. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary. Journal of the American College of Cardiology. 2019 Jun;73(24):3168–209.
7. Lee S-E, Chang H-J, Sung JM, Park H-B, Heo R, Rizvi A, et al. Effects of Statins on Coronary Atherosclerotic Plaques. JACC: Cardiovascular Imaging. 2018 Oct;11(10):1475–84.
8. Endo A. A historical perspective on the discovery of statins. Proc Jpn Acad, Ser B. 2010;86(5):484–93.
9. https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/statins-fact-or-fiction
10. Collins R, Reith C, Emberson J, Armitage J, Baigent C, Blackwell L, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. The Lancet. 2016 Nov;388(10059):2532–61.
11. Wood FA, Howard JP, Finegold JA, Nowbar AN, Thompson DM, Arnold AD, et al. N-of-1 Trial of a Statin, Placebo, or No Treatment to Assess Side Effects. n engl j med. 2020;3.
12. https://en.wikipedia.org/wiki/Nocebo
13. https://manfrommatunga.com/?p=502
14. Danker-Hopfe H, Dorn H, Bornkessel C, Sauter C. Do mobile phone base stations affect sleep of residents? Am J Hum Biol 2012;22:613-618
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.