The Hype and Promise of the Polygenic Risk Score (PRS)
The polygenic risk score may help with personalized prevention, diagnosis and treatment of diseases

Persis, a friend, is of Parsi (Zoroastrian) origin, a community in India that has a higher risk of breast cancer than the general population [1]. Her mother had breast cancer and so did one aunt. She got herself tested for BRCA1 and BRCA2 gene mutations that carry a high risk (50-87%) of developing breast as well as ovarian cancer [2]. Ms. Angelina Jolie has a similar family history of breast cancer and BRCA1 and BRCA2 mutations, for which she had a double mastectomy done, followed 2 years later by oophorectomy (removal of the ovaries), to reduce her risk of breast and ovarian cancer. She explained these decisions of hers in a New York Times opinion piece.
Unlike the Mendelian inherited genetic diseases like thalassemia that I wrote about some time ago, where the presence of one copy (dominant) or two copies (recessive) of the abnormal gene, will always cause the disease to occur, in these “genomic” situations, there is a “risk”, which may either be absolute or relative and may in turn manifest with disease or not. It is likely that Persis would never have landed up with breast cancer, but with a greater than 50% absolute risk, she took an informed decision in conjunction with a geneticist and other experts in breast cancer and then opted to have a double mastectomy.
Genomics therefore, as against “genetics” “is the study not just of single genes but the functions and interactions of all the genes in the genome.” [3]
This post is free to read, but you will need to subscribe with your email ID to read the rest of the post and to listen to the accompanying audio/podcast.
You can listen to the audio/podcast hosted on Soundcloud by clicking the Play button below within the browser itself.
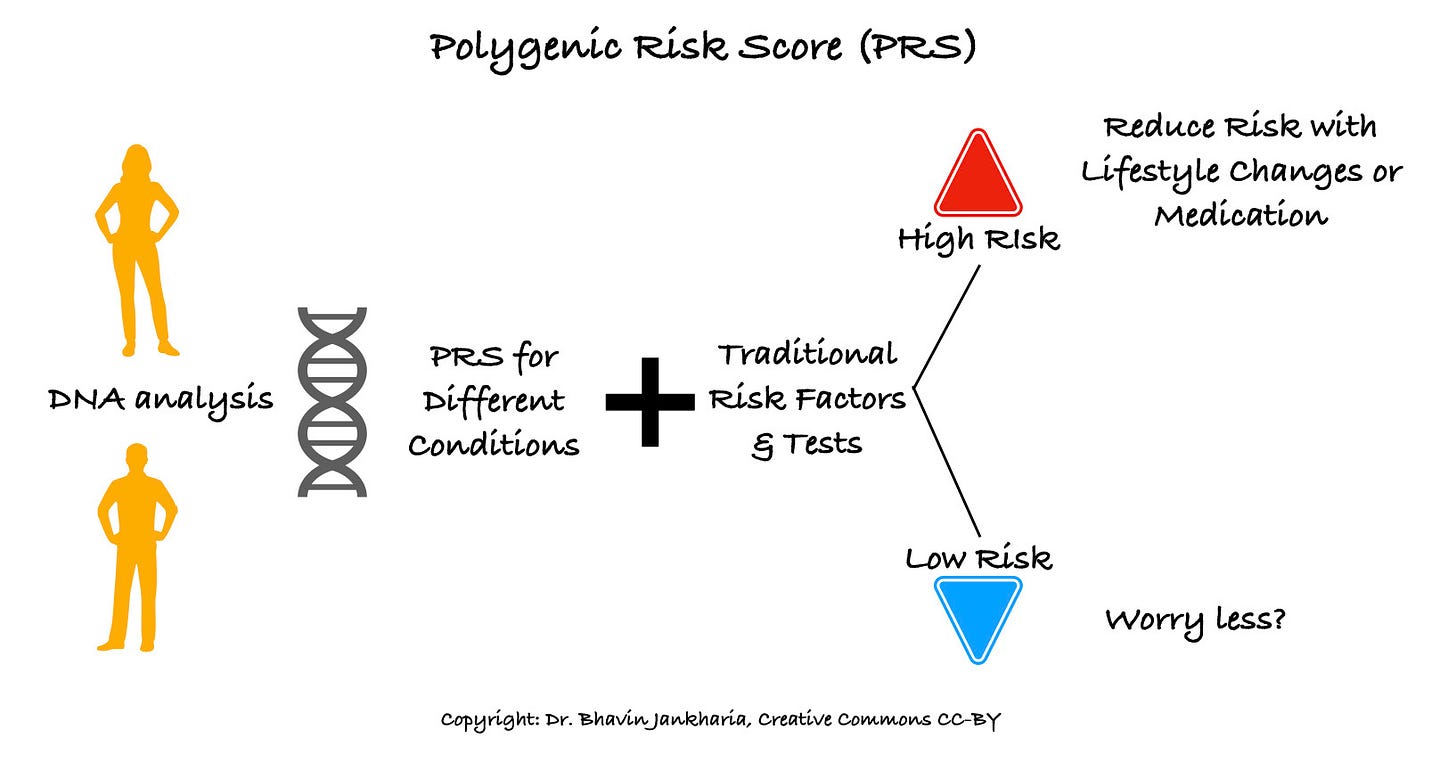
While the promise of genomics has gone through its own crests and troughs, the polygenic risk score (PRS) is creating excitement across multiple branches of medicine. Unlike BRCA1 and BRCA2, which are individual genes (monogenic) that are evaluated to assess risk, in a polygenic risk score, the cumulative risk conferred by mutations in multiple (hence …poly) genes across a person’s genome (hence ...genic) is called the polygenic risk score or PRS [4].
Over the last decade, PRSs have been assessed for many conditions including schizophrenia, coronary artery disease and diabetes [5]. If the score is high, then the premise is that steps could be taken to mitigate the effects of these genetic mutations to reduce risk or hopefully prevent the disease from occurring or like Covid-19 vaccines, reduce the symptoms and severity if the disease does occur.
This postulate also forms the basis of P4 medicine [6]; predictive, preventive, personalized and participatory. There has been considerable excitement about P4 medicine in the fields of engineering, biotechnology, genomic and information technology (IT), given the anticipated promise of genomics to change the way medicine is practiced and to consequently improve overall survival and quality of life, across the globe. Unfortunately, we are not there yet, except in very specific situations like BRCA testing for breast and ovarian cancer, and that too is hardly ever done routinely in India [7].
The ultimate test of the power of a diagnostic study is whether it can change the end-points of either survival or lead to a better quality of life. These studies usually take a long time to come to fruition, something that clearly frustrates engineers and those involved with big data, who believe that it is possible to reduce the time frame of these studies by analyzing large population datasets to get statistical inferences. But statistical and mathematical inferences are no substitutes for on-the-ground, patient and people based clinical data as we have seen with the Covid-19 vaccine trials.
For any PRS to become a routine risk assessment tool, it has to be validated in a trial where the PRS is used to stratify individuals into randomized groups for prevention or treatment as the case may be and the results unequivocally show that basing management decisions on the PRS improves survival or prevents disease. We have a long way to go before such trials and their results come out.
Many start-ups, however are not willing to wait, and are already offering PRSs directly to consumers bypassing traditional medical pathways. If you just Google “polygenic risk score India” you will find such companies.
There are other problems. Most of the data currently available is from European ancestry studies. There been only one study validating a PRS for coronary artery disease in South Asians, and this too is just the first step [8] that now needs clinical validation with a large population based trial.
More alarming is the commercial availability of services in the Western countries that do embryo selection based on the PRSs of the parents, siblings and the embryos, to then choose those embryos with the highest chance of being intelligent or the least risk of developing schizophrenia or coronary artery disease or breast cancer [9]. I can’t even get my head around this, but maybe its just me and the fact that my kids are already past their 20s. Would young parents be willing to do this? I guess so, otherwise I don’t see how these companies could flourish. At this moment in time, in any case, since PRSs for Indian/South Asian ancestry do not exist, this service really cannot be used for and by Indians/South Asians.
On the other hand, you can argue with me that if the goal of atmasvasth is to live long healthy and to have as long a healthspan as possible, then anything we do to be healthy and prevent disease including embryo selection, should be acceptable. After all, if the fetus or embryo has thalassemia major or Down’s syndrome, we anyway don’t implant such an embryo or allow the pregnancy to proceed. Using a PRS to select embryos with the best chance of a good healthspan is then just the next step, isn’t it?
So what is your matka? Your genes and your genome are the matkas you are born with and have no control over in most instances. It is what you get from your parents, unless of course your parents (assuming you are reading this 20 years from now) have pre-selected your genetic profile to give you the best chance of a long healthspan.
In the future, once we have more clarity about PRSs for prevention of disease in those with Indian/South Asian ancestry and there is actual clinical data that using these PRSs does help mitigate risk, it is possible that PRSs, just like our blood sugar, blood pressure, LDL and triglyceride levels, will become routine and commonplace.
Until then, you could just be physically active, eat sensibly and sleep well and use traditional methods to identify risks if any and take steps to reduce these as the case may be.
Footnotes:
1. Yeole BB, Kurkure A, Advani S et al. An Assessment of Cancer Incidence Patterns in Parsi and Non Parsi Populations, Greater Mumbai. Asian Pac J Cancer Prev. 2001;2(4):293-298. PMID: 12718621.
2. Gupta S, Rajappa S, Advani S et al. Prevalence of BRCA1 and BRCA2 Mutations Among Patients With Ovarian, Primary Peritoneal, and Fallopian Tube Cancer in India: A Multicenter Cross-Sectional Study. JCO Glob Oncol. 2021 Jun;7:849-861. doi: 10.1200/GO.21.00051. PMID: 34101484.
3. Guttmacher AE, Collins FS. Genomic Medicine — A Primer. Guttmacher AE, Collins FS, editors. N Engl J Med. 2002 Nov 7;347(19):1512–20.
4. Sugrue LP, Desikan RS. What Are Polygenic Scores and Why Are They Important? JAMA. 2019 May 14;321(18):1820-1821. doi: 10.1001/jama.2019.3893. PMID: 30958510.
5. Slunecka JL, van der Zee MD, Beck JJ et al. Implementation and implications for polygenic risk scores in healthcare. Hum Genomics. 2021 Jul 20;15(1):46. doi: 10.1186/s40246-021-00339-y. PMID: 34284826; PMCID: PMC8290135.
6. Flores M, Glusman G, Brogaard K, Price ND, Hood L. P4 medicine: how systems medicine will transform the healthcare sector and society. Personalized Medicine. 2013 Aug;10(6):565–76.
7. Hunter DJ, Drazen JM. Has the Genome Granted Our Wish Yet? N Engl J Med. 2019 Jun 20;380(25):2391–3.
8. Wang M, Menon R, Mishra S et al. Validation of a Genome-Wide Polygenic Score for Coronary Artery Disease in South Asians. J Am Coll Cardiol. 2020 Aug 11;76(6):703-714. doi: 10.1016/j.jacc.2020.06.024. PMID: 32762905; PMCID: PMC7592606.
9. Turley P, Meyer MN, Wang N et al. Problems with Using Polygenic Scores to Select Embryos. N Engl J Med. 2021 Jul 1;385(1):78-86. doi: 10.1056/NEJMsr2105065. PMID: 34192436.
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.

