The Matka of Our Genes
The matka of our genes. Genes matter

Genetics
Kavita is thalassemia minor positive, diagnosed on a routine screening test almost a quarter century ago. She had an arranged marriage with Sanjay, who was also screened in the period between the engagement and the wedding and was found to be normal, not carrying the thalassemia gene.
This post is free to read, but you will need to subscribe with your email ID to read the rest of the post.
Thalassemia is a blood disorder where the beta-globin part of the hemoglobin (Hb) that carries oxygen in the blood is absent. This leads to an increase in the alpha-globin chains causing poor production of red blood cells (RBCs) and peripheral hemolysis (destruction) of these RBCs, which in turn leads to anemia and other problems. Without treatment, survival is at best 10 years or so. Treatment typically consists of regular, life-long blood transfusions, at two-three weekly intervals, along with drugs to remove the excess iron that gets deposited in the body as a result of these blood transfusions. With proper treatment, these days, thalassemia patients often live into their 40s and 50s. Other forms of treatment are allogenic stem cell transplantation and gene therapy, discussed below.
Thalassemia is an inherited genetic abnormality that is autosomal recessive, which means that the person has to have two copies of the abnormal gene to get the disease, as against autosomal dominant disorders (like Huntington chorea or neurofibromatosis 1) where only one copy of the gene from either parents is needed. Autosomal conditions are those that involve genes on the 22 chromosomes while X-linked conditions (hemophilia A) are those that are transmitted through the X-chromosome, which is a sex-determining chromosome. (All humans have 23 chromosomes, the 23rd being the sex chromosome, X in men and Y in women).
A thalassemia minor patient has a mild abnormality of the Hb that does not interfere with day to day life or survival, but the Hb level in the blood rarely goes above 11.5 or 12 mg/dl. Normal people have values of 13-14 mg/dl. If both parents are thalassemia minor gene positive, then there is a 50% chance that the child will also inherit the thalassemia minor gene, a 25% chance that the child will get both abnormal genes and hence have thalassemia major and a 25% chance that the child will be absolutely normal. If one parent is a minor and the other normal, then the child has a 25% chance of carrying the abnormal gene.
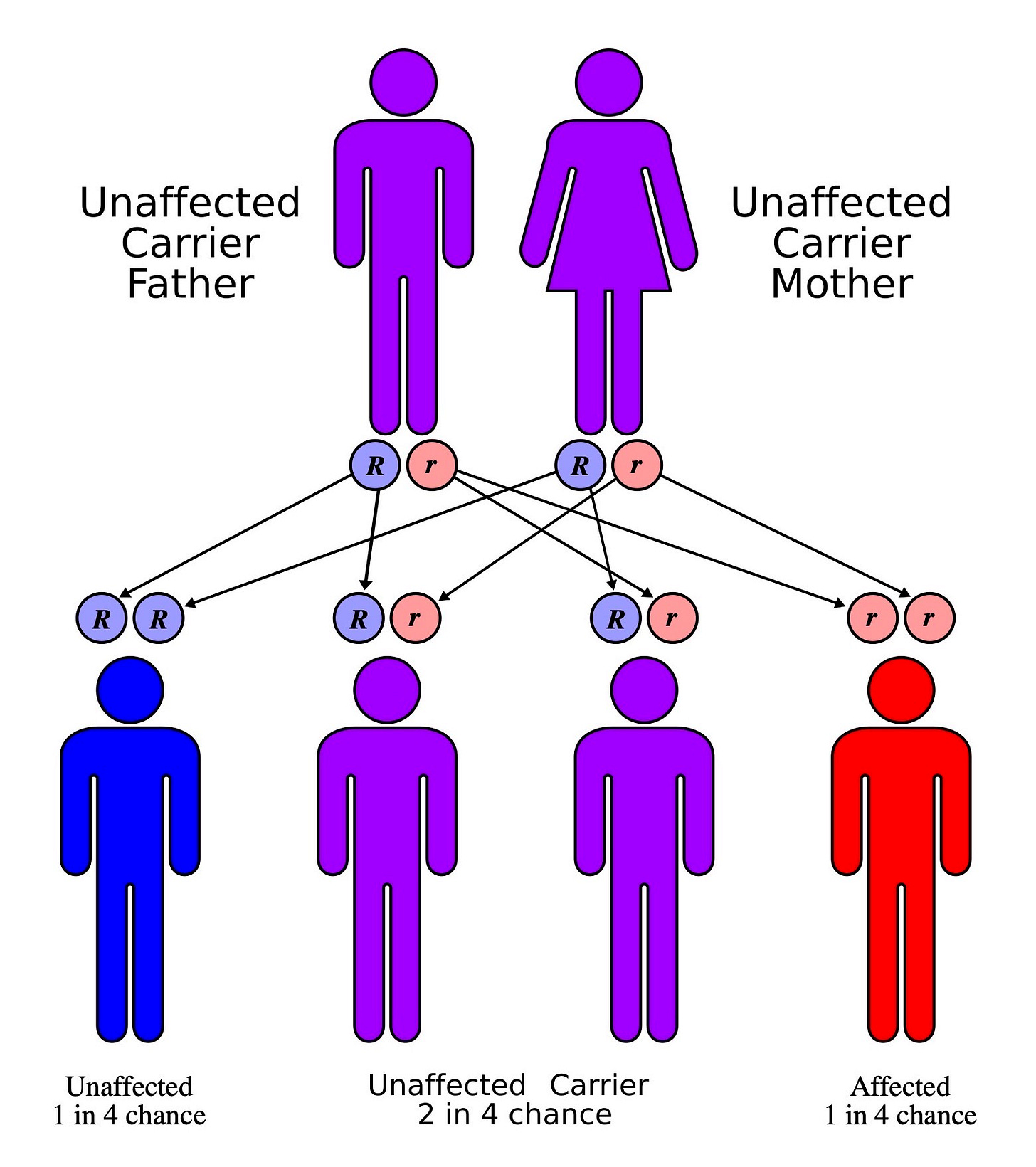
Fig. 1: By en:User:Cburnett - Own work in Inkscape, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=1840082
The best way to prevent thalassemia major is for two thalassemia minor carriers to not marry or procreate. If they do so for any reason, then in the early stages of pregnancy, amniotic or chorionic villus sampling from the mother’s uterus needs to be performed to determine whether the fetus is normal, minor or major. If major, then this is an indication for premature termination of pregnancy.
This also means that whenever a thalassemia minor person decides to get married or bear children, the partner has to be screened for the thalassemia gene.
Kavita became pregnant and everything was going well. But, when their first baby Sheena was born, disaster struck. She turned out to be thalassemia major. This meant that Sanjay was thalassemia minor positive after all.
They got him re-tested. He was positive for the thalassemia minor gene.
The first lab had somehow screwed up the result and given him a normal report. As a result, Kavita and Sanjay did not bother to get genetic testing done to check Sheena’s status during pregnancy. Sheena is a lovely, pretty, joyous girl. Now 27 years old, she has to take blood transfusions every month and drugs to reduce the iron overload in other organs of the body and while she is otherwise normal, it is virtually impossible for her to find someone to marry.
One wrong laboratory test and this is the matka for Sheena and her parents and the rest of the family as well.
Thalassemia is an example of a genetic Mendelian disorder, as against genomic disorders, which we will discuss in a another post. Genetics is the study of single genes and their effects [1] and genetic disorders follow simple rules based on inheritance patterns. They are not common, but when applied to a large population like India, the numbers can eventually become staggering and unmanageable. Around 10,000 to 12,000 babies with thalassemia major are born annually [2]. This translates to a figure of 1 thalassemia major patient in 2250 live births, assuming 27 million live births in India, which leads to a prevalence of almost a 100,000 thalassemia major patients in the country, requiring blood transfusions every 2-3 weeks…this can easily and in fact does overwhelm our public health system and many thalassemics depend on charities and social institutions to help them out, especially since the vast majority come from a poorer socio-economic background. During the early part of the current pandemic, many thalassemics had no access to their regular blood transfusion centres and many of them ran into significant trouble [3].
India's Covid-19 epidemic is rolling back decades of progress made in fighting other diseases - from thalassemia to cancer to malaria.
— Joe Wallen (@joerwallen) September 30, 2020
@M_S_Alam111 and I met one woman in Jharkhand whose son tragically died in her arms outside an empty blood bank.https://t.co/rnlxMhQlw1
7 year old Randip, son of daily wagers,was scheduled for a blood transfusion. Now he's turned away from this COVID-only hospital. He suffers from Thalassemia which can reduces life span to 25-30 years if not treated properly. Where will India's non-COVID poor go? My #Mojo report pic.twitter.com/RivGpk6x8c
— barkha dutt (@BDUTT) April 14, 2020
The definitive form of treatment is allogenic hematopoietic stem cell transplantation [4,5], which is expensive (Rs. 15 to 25 lakhs) [6], though there are centres in India in the public sector that perform this procedure if a donor match for the transplantation can be found. Recently, a unique gene therapy has been discovered that also cures thalassemics but is again not affordable for the vast majority of patients in India [7], costing more than 1 million dollars (7.5 crores), even if available. While prevention is the best method, the low education levels in the populations at risk and the inability to get to the villages for genetic screening are major challenges that are difficult to overcome in our country.
Funnily, thalassemia evolved as nature’s response to malaria [8] almost 100,000 years ago in Africa, where it was and is still endemic. The thalassemia gene along with others like the sickle cell gene, protect against malaria, which at that time was perhaps a bigger issue than the anemia and other problems that thalassemia brings.
#Thread :
— Dr. Pradeep Gadge 🇮🇳 (@Dr_Gadge) December 13, 2019
In 1949, British scientist John Burdon Sanderson Haldane made a novel connection between red cell disorders & malaria. #FactfulFriday #Facts #DidYouKnow #Thalassemia #Malaria #DrGadge pic.twitter.com/JpRMF9XFng
There are so many matkas here that affect Sheena apart from just her genes and the laboratory. mess-up. Our body’s fight against malaria tens of thousands of years ago is linked to Sheena’s predicament today. The Indian government does not have a funding program to help her with definitive treatment. Sheena herself is unable to afford either stem cell transplantation or gene therapy and hence will continue to endure the blood transfusions once every 3 weeks and take regular medication for iron chelation.
Similar stories abound for other types of genetic Mendelian disorders, the vast majority of which are listed at omim.org, a repository for all monogenic disease related research [9]. The other common conditions seen in India are sickle cell anemia, cystic fibrosis, spinal muscular atrophy (SMA) and hemophilia.
Last year, Novartis announced a gene treatment for SMA that has worked for up to 5 years currently in the first subjects where it has been used [10]. The cost of treatment is 2.1 million dollars in the US (approx. 14.5 crores), but Malachi Anderson, who was a test subject was lucky to get the treatment free and is today an alive and kicking 5-years old child.
If however, Malachi were to be born in a poor country, like Aarav, who died recently [11], not able to get funding for the treatment (now Rs. 5 crores or so), or were to born just two years prior to the announcement of the treatment (survival is generally around 2 years), or did not have access to the clinical trial for whatever reason, then he would not be alive. A campaign recently highlighting Aarav’s and Teera Kamat’s plight did help…the Govt waived off all duties on the drug…but that is still not enough given the price, which is pretty much unaffordable by almost anyone in our country.
Baby Aarav sufferin frm #SpinalMuscularAtrophy same as #TeeraKamat passed away today Selective help in few cases won’t help patients & parents @curesmaindia have been requestin @Dev_Fadnavis @PMOIndia @narendramodi to help us Win #battleagainstsma 5 SMA Type 1 are on life support pic.twitter.com/VnKPMcKYvC
— Alpana Sharma (@alpanaS16) February 12, 2021
How does this matka of your genes affect you? If you have a genetic disorder or live with someone who suffers from one that needs expensive or lifelong treatment, the challenges are enormous…whether it is just simple survival, or the expenses involved. Even if you are rich and have access to resources, the poor state of our healthcare is still a marked adverse matka.
Footnotes:
1. Guttmacher AE, Collins FS. Genomic Medicine — A Primer. Guttmacher AE, Collins FS, editors. N Engl J Med. 2002 Nov 7;347(19):1512–20.
2. Colah R, Italia K, Gorakshakar A. Burden of thalassemia in India: The road map for control. Pediatric Hematology Oncology Journal. 2017 Dec;2(4):79–84.
4. Srivastava A, Shaji RV. Cure for thalassemia major - from allogeneic hematopoietic stem cell transplantation to gene therapy. Haematologica. 2017 Feb;102(2):214-223. doi: 10.3324/haematol.2015.141200
5. Baronciani D, Angelucci E, Potschger U, Gaziev J, Yesilipek A, Zecca M, et al. Hemopoietic stem cell transplantation in thalassemia: a report from the European Society for Blood and Bone Marrow Transplantation Hemoglobinopathy Registry, 2000–2010. Bone Marrow Transplant. 2016 Apr;51(4):536–41.
6. Sharma SK, Choudhary D, Gupta N, Dhamija M, Khandelwal V, Kharya G, Handoo A, Setia R, Arora A. Cost of hematopoietic stem cell transplantation in India. Mediterr J Hematol Infect Dis. 2014 Jul 1;6(1):e2014046
7. Thompson AA, Walters MC, Kwiatkowski J, Rasko JEJ, Ribeil J-A, Hongeng S, et al. Gene Therapy in Patients with Transfusion-Dependent β-Thalassemia. New England Journal of Medicine. 2018 Apr 19;378(16):1479–93.
8. Kumar R, Sagar C, Sharma D, Kishor P. β-Globin Genes: Mutation Hot-Spots in the Global Thalassemia Belt. Hemoglobin. 2015 Jan 2;39(1):1–8.
9. Amberger JS, Bocchini CA, Scott AF, Hamosh A. OMIM.org: leveraging knowledge across phenotype–gene relationships. Nucleic Acids Research. 2019 Jan 8;47(D1):D1038–43.
11. https://www.mid-day.com/mumbai/mumbai-news/article/covid-19-mumbai-records-over-500-cases-for-third-consecutive-day-23159617
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.

