The Matka of Covid-19 Treatment in India - "Cheap?" - Not Really!!
Individual tests may be cheap, but the overall cost of "treatment" of minimally symptomatic to asymptomatic Covid patients is higher than in the US

With a lot of help from Dr. Akshay Baheti @Dr_AkshayBaheti. Thanks Akshay
A recent paper [1] on antibiotic usage has shown that many low and middle income countries (LICs and LMICs respectively) like Vietnam and Bangladesh (and India) which traditionally are supposed to have poor antibiotic availability and hence suboptimal treatment of infections, actually have the opposite problem. Paradoxically, many antibiotics are quite easily available directly from pharmacies, they are often taken at the first instance of fever and frequently without doctor prescriptions and without the doctor(s) involved. It is this widespread, irrational use of antibiotics that is likely the cause of the increasing antibiotic resistance in these geographies including our country and the reason why patients can directly access these antibiotics is because they are extremely cheap and affordable compared to their price in high income countries (HICs) and regulatory oversight on their sale and availability is virtually non-existent.
This post is free to read, but you will need to subscribe with your email ID to read the rest of the post and to listen to the accompanying audio/podcast.
You can listen to the audio/podcast hosted on Soundcloud by clicking the Play button below within the browser itself.
There is no question that the lower cost of many initially expensive drugs has made a world of a difference to the management of conditions like HIV, tuberculosis and other chronic diseases and saved countless lives. India has been a pioneer in manufacturing and even exporting these low-cost drugs to other LICs and LMICs. But it is precisely this low cost of prescription drugs that has the potential for overuse/abuse.
A case in point is a drug like pirfenidone [2] which has brought a ray of hope to patients with fibrotic interstitial lung disease, who otherwise have dismal prognosis and survival (just 3-5 years for idiopathic pulmonary fibrosis (IPF)). But because pirfenidone costs just around Rs. 150-Rs.200 per day, which is 10-100 times lower than the cost in many other countries, it is used indiscriminately in any patient with any kind of diffuse lung disease, including experimentally, without any evidence, in Covid-19 patients, apparently to prevent lung fibrosis…with all its attendant complications.
This cost differential between India and other countries translates into something quite interesting when it comes to the management of asymptomatic or minimally symptomatic patients with Covid-19.
80% of patients with Covid-19 have asymptomatic to minimally symptomatic disease. In most parts of the Western world, patients with asymptomatic to minimally symptomatic Covid-19 are asked to stay at home, take paracetamol or ibuprofen for fever, perhaps a cough suppressant if needed, maintain adequate nutrition and hydration, isolate themselves, take steps to prevent spread of infection to others and check their oxygen (O2) saturations regularly with a pulse oximeter. There are constantly updated guidelines that help the patients and doctors understand management strategies and protocols, e.g. the BMJ protocols in the UK or the NIH guidelines in the United States. If we Google for Indian guidelines, they are difficult to find...but finally the AIIMS/ICMR guideline chart was updated two days ago (Fig. 1)
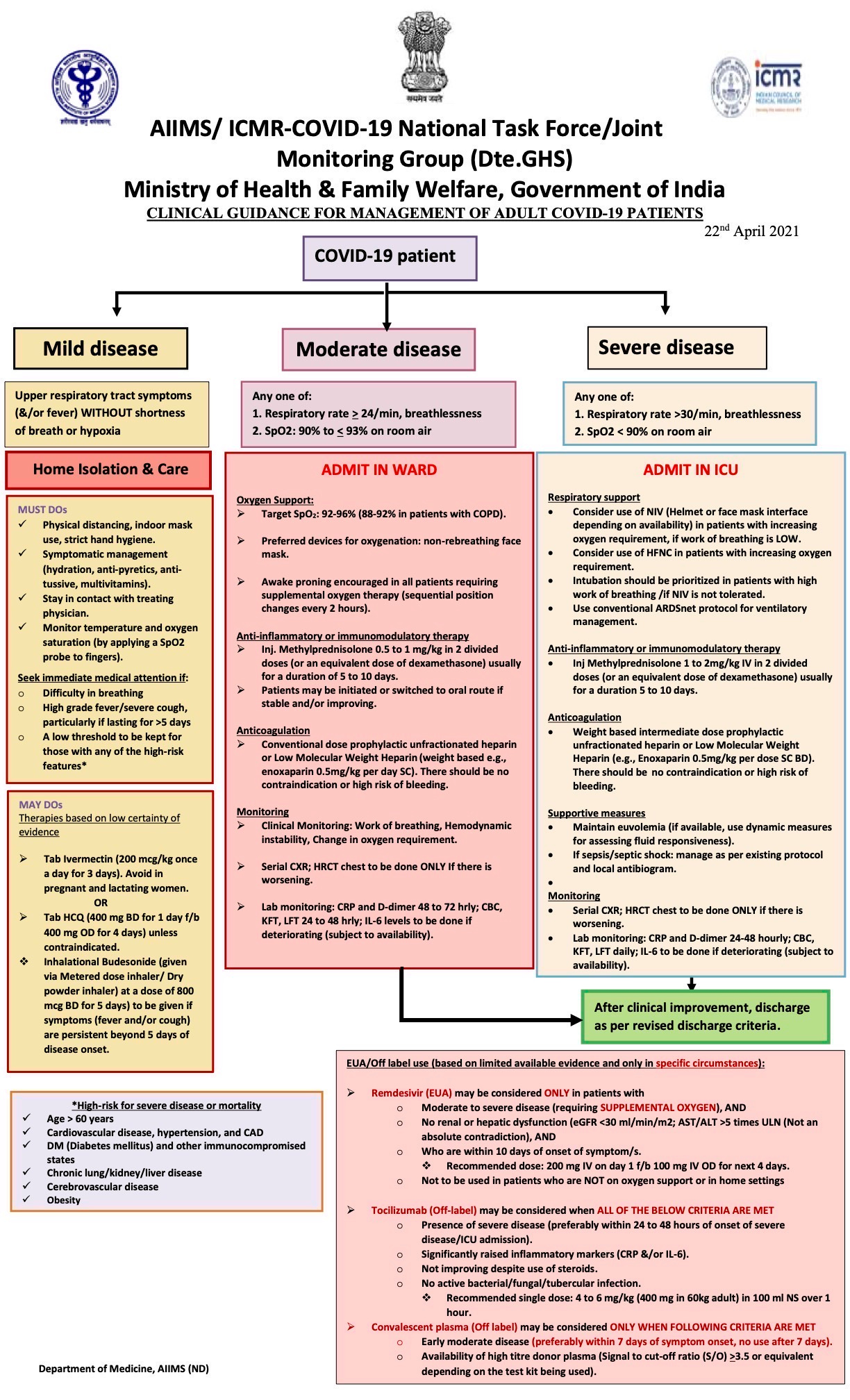
Guidelines such as these are not easily available to the public or even doctors and seem to primarily rely on WhatsApp for dissemination and since WhatsApp has no filters to decide what is correct or not or “official” or not, there are multiple confusing strategies being used across the country including the one I spoke and wrote about in “The Matka of “Doing Something”, where Dr. Saurabh Jha from the US tweeted about the long list of diagnostic tests and drugs that a 15-year old patient in New Delhi, with only fever, had received.
Individually, these drugs and tests cost much less than in other parts of the world (e.g. a CT scan of the chest can be done for as low as Rs. 2000 in India, but if paid for upfront may cost Rs. 50,000 to Rs.70,000 in the US). But when so many of them are prescribed together, the costs add up.
Let’s look at a comparative table of tests and prices for an asymptomatic or minimally symptomatic person with Covid-19 in India and USA (Fig. 2).
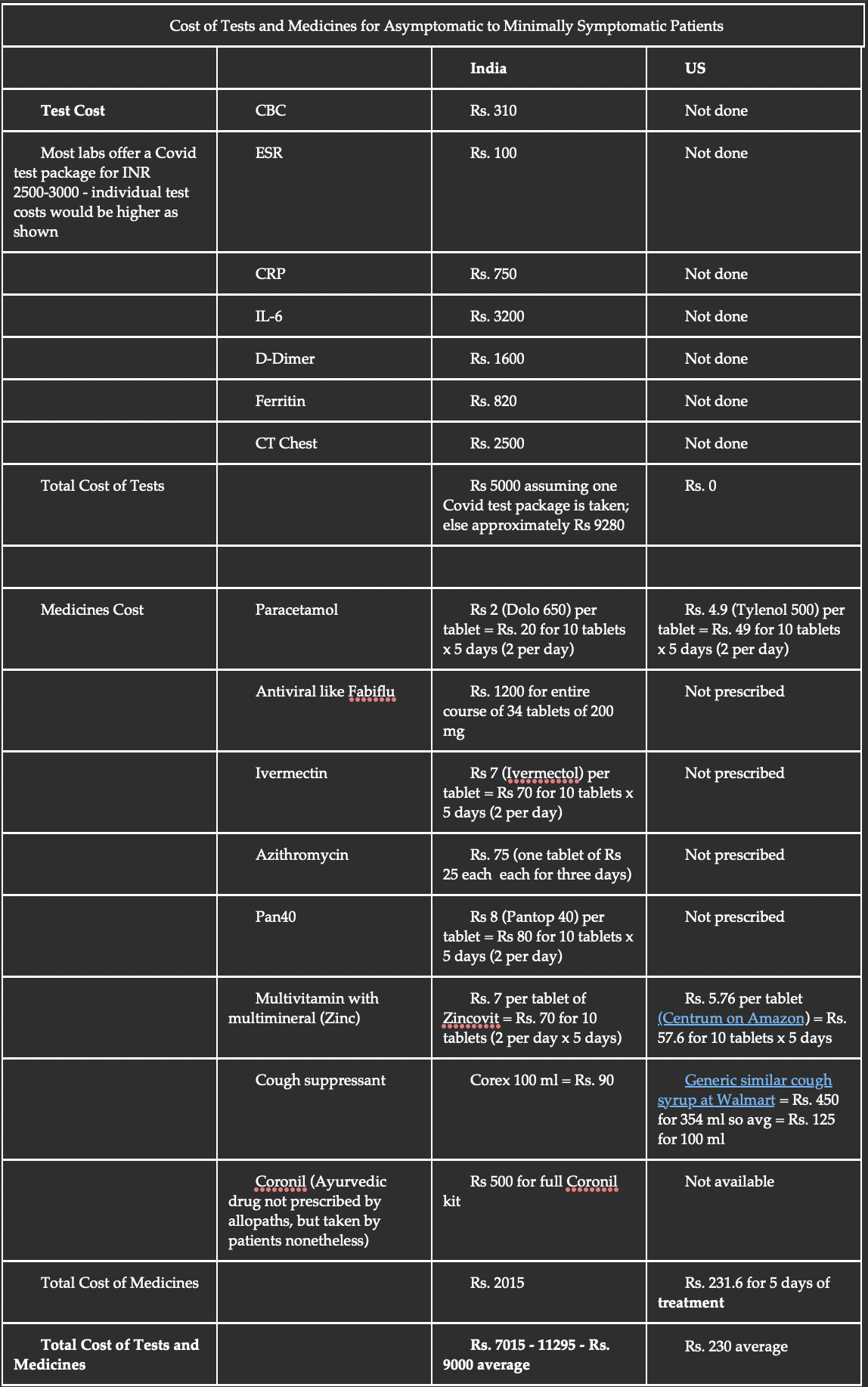
(Compiled by Dr. Akshay Baheti and Dr. Bhavin Jankharia. We have not included the price of a pulse oximeter, since they are often used by an entire family - the prices are however comparable. Doctor consultation and RT-PCR test costs are not included, because these differ widely based on availability of insurance or not and are not relevant to this discussion).
Now let’s look at income. The per capita income in India in FY 20 was Rs. 11,254, while the per capita median income was Rs. 2.24 lakhs in the US in 2019, which is an approximately 20 times difference (the values are different if we look at GDP per person based on purchasing power parity, but that does not apply here).
Look at the irony. An average Indian, if asymptomatic or minimally symptomatic with Covid-19, spends 39 times more for diagnosis and treatment while earning 20 times less than someone similar in the US. If a family of four is infected together, which is quite the norm these days, they would land up spending around Rs. 36,000 to Rs. 40,000 at one go, without taking into account doctor consultation fees, transportation and other similar costs.
The issue is that even if we assume that all the tests and drugs are justified based on the doctors’ clinical judgment or the new mutant strain or because Indians are different from people in the West, we as a country, can ill-afford an expense that comes to 81% of an average Indian’s monthly income, compared to an expense that is just 0.1% of the monthly income of an average American (Fig. 3). This just further reinforces our quadruple Indian adverse healthcare whammy.
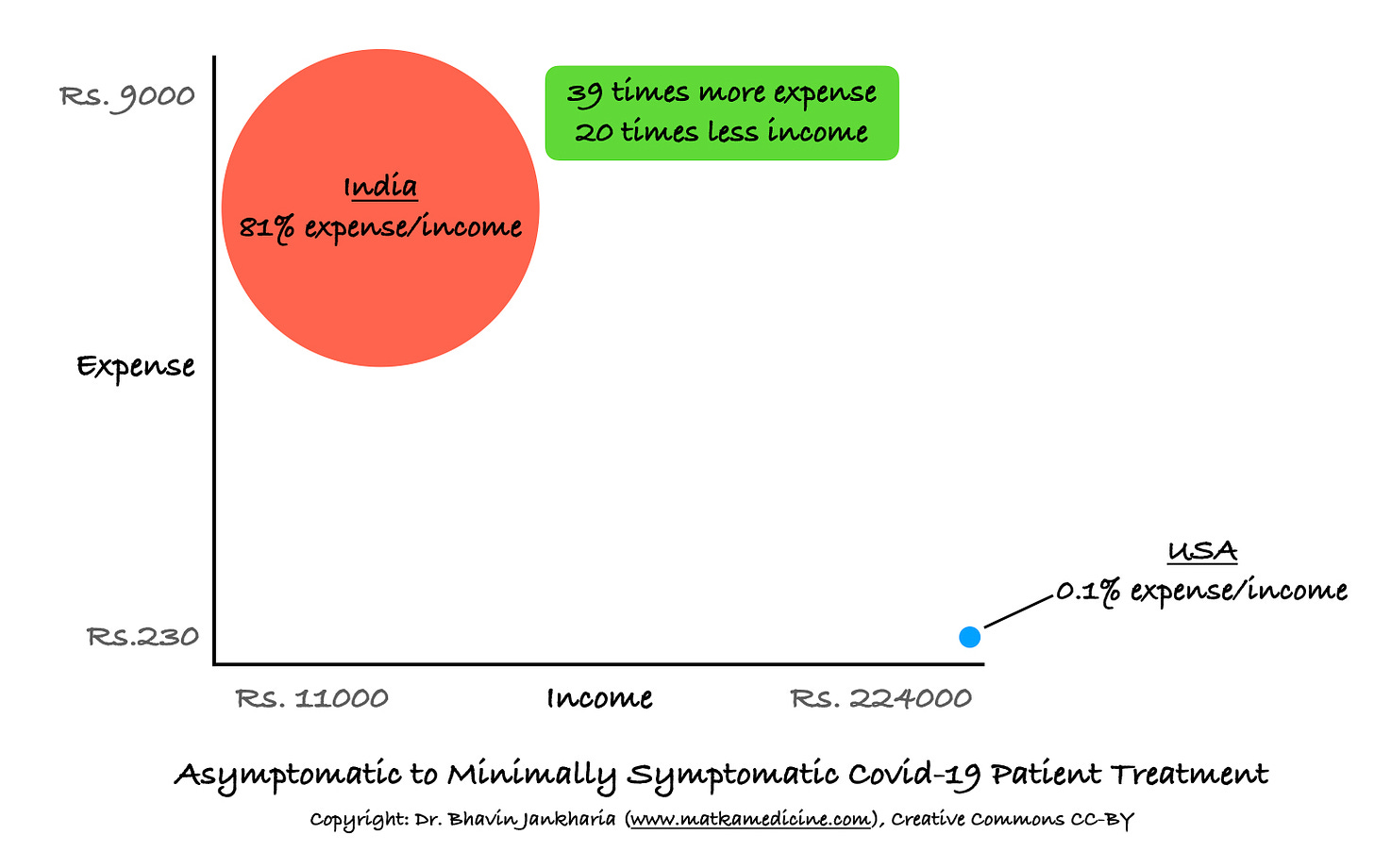
Everyone wants the best for themselves and their family, which means that every patient who is prescribed these tests and drugs, will get them done, irrespective of whether they can afford them or not. This can easily become a catastrophic expense and push people into poverty, especially when many of them have already lost income due to Covid-19 itself. Every year, around 50 million (5 crore) Indians fall back into poverty because of some kind of catastrophic health expenditure and this number is likely to increase due to Covid-19, given that 60% of health expenditure in our country is out of pocket. And we are not even talking of expenses in those with moderate to severe disease who need hospitalization and are prescribed drugs like remdesivir or tocilizumab or plasma therapy whether they are needed or not or work or not.
What is your matka here? Do we really have to really spell that out? If you live in India, and are minimally symptomatic or asymptomatic with Covid-19, you will land up paying much much more than your counterpart in the US (justified or not is not the issue here). This may dent your income significantly depending on who you are and can even start a slide into poverty due to the catastrophic expense (compared to income) that this may entail.
Footnotes
- Do NTT, Vu HTL, Nguyen CTK, Punpuing S, Khan WA, Gyapong M, Asante KP, Munguambe K, Gómez-Olivé FX, John-Langba J, Tran TK, Sunpuwan M, Sevene E, Nguyen HH, Ho PD, Matin MA, Ahmed S, Karim MM, Cambaco O, Afari-Asiedu S, Boamah-Kaali E, Abdulai MA, Williams J, Asiamah S, Amankwah G, Agyekum MP, Wagner F, Ariana P, Sigauque B, Tollman S, van Doorn HR, Sankoh O, Kinsman J, Wertheim HFL. Community-based antibiotic access and use in six low-income and middle-income countries: a mixed-method approach. Lancet Glob Health. 2021 May;9(5):e610-e619. doi: 10.1016/S2214-109X(21)00024-3. Epub 2021 Mar 10. PMID: 33713630.
- King TE Jr, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, Gorina E, Hopkins PM, Kardatzke D, Lancaster L, Lederer DJ, Nathan SD, Pereira CA, Sahn SA, Sussman R, Swigris JJ, Noble PW; ASCEND Study Group. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014 May 29;370(22):2083-92. doi: 10.1056/NEJMoa1402582. Epub 2014 May 18. Erratum in: N Engl J Med. 2014 Sep 18;371(12):1172. PMID: 24836312.
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.